The human body's interaction with extreme cold presents unique medical challenges that often go overlooked in everyday safety discussions. While frostbite remains the most widely recognized cold-related injury, a lesser-known but equally dangerous phenomenon called localized cryogenic burns (or cold burns) poses significant risks in both industrial and domestic settings. These injuries occur when skin or underlying tissues freeze upon contact with supercooled surfaces or substances, triggering cellular damage that mirrors thermal burns in both appearance and healing complications.
Unlike generalized hypothermia which affects the entire body, localized cryogenic burns target specific areas - typically the hands, face, or any exposed skin that makes direct contact with freezing materials. The injury mechanism involves ice crystal formation within cells, which ruptures membranes and disrupts blood flow. What makes these injuries particularly insidious is their deceptive onset; victims often don't immediately recognize the damage because cold numbs nerve endings. By the time pain signals emerge, tissue destruction may already be substantial.
Industrial environments harbor numerous cryogenic burn hazards that workers frequently underestimate. Liquid nitrogen (-196°C), dry ice (-78.5°C), and compressed CO2 all present substantial risks during handling. The aerospace industry faces particular challenges when working with cryogenic fuel components, while food processing plants using flash-freezing technologies report some of the highest incidence rates. Even brief contact with uninsulated pipes carrying refrigerants can cause immediate freezing of epithelial layers.
Medical professionals observe that cryogenic burns often present with distinct progression patterns. The affected area typically appears waxy and pale during initial exposure, later developing clear demarcation lines similar to thermal burns. As tissues thaw, severe edema and blistering occur, sometimes accompanied by compartment syndrome in deeper injuries. Unlike heat burns which trigger immediate inflammatory responses, the delayed reaction in cold burns frequently leads to underestimation of injury severity during initial triage.
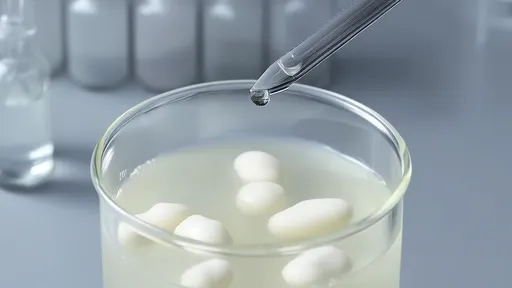
Treatment protocols for cryogenic burns require specialized approaches that differ from both thermal burn care and frostbite treatment. Rapid rewarming in water baths maintained at 40-42°C (104-107.6°F) remains the gold standard, but this must be carefully controlled to avoid additional tissue damage. The rewarming process itself often proves intensely painful, requiring substantial analgesia. Perhaps most counterintuitive to first responders is the critical prohibition against rubbing affected areas - a common instinct that can exacerbate cellular damage in frozen tissues.
Preventive measures in occupational settings demand rigorous engineering controls and personal protective equipment (PPE) standards. Insulated gloves rated for cryogenic exposure, face shields, and specialized aprons constitute minimum requirements when handling extremely cold materials. Safety training must emphasize that ordinary winter gloves provide virtually no protection against industrial cryogens - a dangerous misconception that contributes to many preventable injuries. Engineering solutions like vapor barriers and automated handling systems have proven effective in reducing direct contact scenarios.
The long-term consequences of cryogenic burns often surprise patients during recovery. Many experience lasting neuropathic pain or abnormal cold sensitivity in affected areas, sometimes persisting for years. Severe cases may require surgical debridement or even amputation when deep tissue necrosis occurs. Rehabilitation frequently involves desensitization therapy and careful monitoring for late-onset complications like fibrosis or contractures that can impair mobility.
Emerging research suggests certain populations face elevated risks from cryogenic exposure. Diabetic patients with peripheral neuropathy prove particularly vulnerable due to diminished sensation in extremities. Similarly, individuals taking beta-blockers or other medications that affect peripheral circulation may sustain more severe injuries from identical exposures compared to healthy counterparts. These findings have prompted calls for enhanced medical screening in occupations involving cryogen handling.
Public awareness campaigns struggle against widespread misconceptions about cold injuries. Many people mistakenly believe that brief contact poses minimal risk, unaware that certain cryogens can cause irreversible damage in under five seconds of exposure. Educational initiatives now emphasize the "triple threat" of cryogens - their ability to freeze tissue, displace oxygen, and create high-pressure hazards simultaneously. This holistic understanding proves crucial for developing proper respect for these materials without fostering counterproductive fear.
Technological advancements continue reshaping cryogenic safety landscapes. New phase-change materials in PPE offer improved protection while maintaining dexterity, a critical factor for precision work. Thermal imaging systems now help safety officers detect developing cold injuries before visible symptoms appear. Perhaps most promising are the bioengineered skin substitutes specifically designed for cryogenic burn treatment, showing remarkable success in preserving tissue viability when applied during early treatment phases.
The medical community increasingly recognizes cryogenic burns as a distinct injury category requiring specialized protocols. Current research focuses on improving early diagnostic methods, including biomarkers that might predict tissue salvageability. Meanwhile, occupational safety organizations worldwide are working to standardize training programs and equipment specifications for cryogen handling - an overdue development given the expanding use of ultra-cold technologies across multiple industries.
As liquid natural gas becomes more prevalent in energy sectors and cryogenic applications expand in high-tech fields, understanding localized freezing injuries grows increasingly vital. What was once considered a niche occupational hazard now demands broader recognition in both medical practice and public safety education. The complex pathophysiology of these injuries continues to challenge clinicians while driving innovation in both treatment and prevention strategies.

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025
By /Aug 6, 2025
By /Aug 6, 2025

By /Aug 6, 2025

By /Aug 6, 2025